by Jeremiah Escajeda, MD FAEMS
Our world has changed and, according to public health experts in the US, it will never be the same.
EMS continues to staff the front lines of our new reality.
As local, national and international COVID-19 epidemiological data transforms daily, so do our local EMS protocols, policies and processes, compounding the stress that EMS professionals and first responders endure. We are in “disaster mode” as a speciality. The current pandemic has disrupted everything; our mental edge going to-and-after work, how we interact with patients and colleagues, our friends and our family.
Some of our geographical regions are fortunate enough to not suffer the severe burden of the overwhelming influx of COVID-19 patients to our healthcare systems as hot spots in New York City already have. We have, however, changed as an international speciality, forever, because of the pandemic. The situation will continue to evolve, but the future holds many uncertainties.
The COVID-19 pandemic presents additional challenges in our EMS community. A term we would like to call the Collateral COVID-19 Damage. (#CollateralCovidDamage). On one side, we have the physical and mental health ramifications of responding as frontline workers, on the other, the medical interventions that we deliver to all patients have changed.
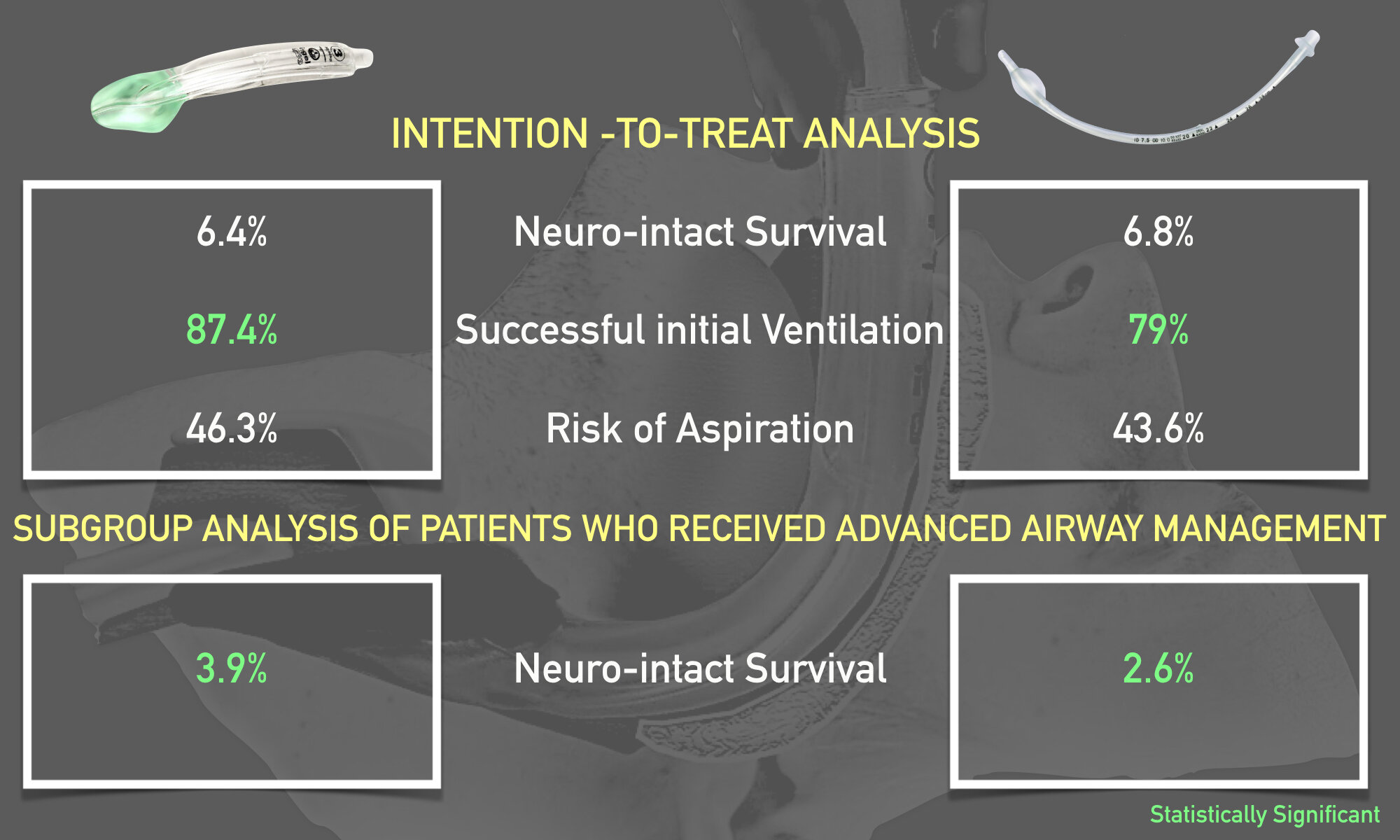
Consider three months ago. You and your partner arrive on-scene, mask-free, to an elderly patient with respiratory failure from a nursing facility who had a past medical history of decompensated heart failure and was discharged from the hospital for heart failure 7 days ago. She is hypertensive and hypoxic. What would you have done? Administer some nitroglycerin and place the patient on non-invasive positive pressure ventilation (NIPPV) without hesitation.
Now, consider that same patient scenario today.
Are you wearing the correct personal protective equipment (PPE)? Did the PPE policy change? Did you remember to check your email for updates today? Does your agency have enough PPE? What if you are practicing in a COVID-19 hotspot? What if now your agency doesn’t allow NIPPV because of the aerosolization risk of novel coronavirus-19? What do you do with the “Do Not Intubate” status of this patient? What if this nursing facility recently had 15 positive COVID-19 cases? Should this patient be transported? What do you ask or tell the nursing facility staff members who you know are also scared about their other patients, themselves and their families? What do you tell the patient or the family (although it is likely that they won’t be present because of the COVID-19 visitor restrictions, at the nursing facility, during transport and in the hospital)? Can this patient call family members? Did you write down a phone number for their family? What if the receiving facility does not permit prehospital NIPPV from EMS because of the potential risk to hospital staff? Should you forgo NIPPV altogether, for all patients? You hear wheezing, but albuterol nebulizers are bad right? Your partner confirms this. Did you just touch your face? Do you have enough disinfectant to use at the station? At your house? What if you know that if you transport this patient that they may be intubated, without family present? What if they die alone? What if this was a 40-year-old, because you heard on the news that 40-30-20-year-olds are dying from COVID-19? What is this anti-malaria medicine everyone keeps talking about? What do you do before you go home to disinfect? What do you tell your family? What should you share with them? And what if we could just go back to three months ago?
This is the collateral COVID-19 damage.
Having a brain full of these questions is real and it is a normal response to our chaotic, strange world and can be cognitively overwhelming. Just as we can’t go to the grocery store without a mask and a pocket full of sanitizing wipes, we can’t go to a ‘run of the mill’ EMS call without having COVID-19 concerns. This is the new normal for us, for now, but there is hope.
State-based mitigation strategies are working. Communities, while physically distancing, are socially rallying for all frontline workers. Think about how many “thank yous” or “how are you doings” you have been hearing in recent weeks. The free coffee, food, it all helps to mitigate our own collateral covid-19 damage. What you do is valued and critical to combating this pandemic. What you do matters.
We would like to open the post up for you. Give us an example of how you have found meaning or reaffirmation in your work in these difficult times. Share a positive experience that you have encountered in the last few weeks as a frontline worker. Either post here - or if you want - e-mail a sound or video clip, or a written story, to [email protected].
We will combine these into a follow-up post in the coming month.