by Mark Liao, MD, NRP (@EMSDocMark)
Expert Peer Review by Dorothy Habrat, MD (@EMSDrDorothy)
Clinical Scenario
A 25-year-old male is brought to your Finish Line medical station. Bystanders noted that he was unsteady on his feet while running a half-marathon before he collapsed. The outside conditions are notable for an air temperature of 22.7 °C (73 °F) and a humidity of 45%, which subjectively feels quite mild to you. The patient does not respond to questions properly, is pale and diaphoretic. Once inside the medical station tent, his skin does not feel hot when his forehead is touched and is otherwise moist. A tympanic membrane thermometer registers an aural temperature of 36.7 °C (98 °F). The patient is persistently confused and a rectal thermometer is subsequently utilized, which registers 41.1 °C (106 °F).
Review
Exertional Heat Stroke (EHS) is an environmental medical emergency from excessively high body core temperature due to physical exertion. National surveillance data for annual prevalence is difficult as these cases are included with classic heatstroke seen in the elderly [1] or reported alongside other types of exertional heat illness such as heat exhaustion [2,3]. Typical risk groups for EHS include athletes (particularly high school football players [4]) and military personnel. In 2018, the US Armed Forces experienced 578 cases of EHS for soldiers on Active Duty during global operations and training [5] . EHS is also a particular concern for medical planners involved in large sporting events: an 8-year study at the Indianapolis Mini Marathon identified 32 cases of EHS among over 235,000 combined participants [6]. Recognizing the need for early and aggressive treatment of EHS, the National Association of EMS Physicians published an important consensus statement in 2018 that outlines the identification and management of EHS in the pre-hospital setting which will be reviewed here [7].
Identification of EHS
While Exertional Heat Stroke is typically associated with hot conditions, it can still occur in cooler climates.
EHS should be considered if an individual has been performing physical activity and experiences central nervous system disturbance. This can range from irritability or confusion to decreased level of consciousness. Delays in EHS recognition are multifactorial. Counterintuitively, EHS can still occur in cooler weather despite its association with hot climates [8]. It is a common misconception that EHS patients will have stopped sweating. Patients, when touched, may not always feel warm and may even feel cool with skin moisture present.
Waiting for the development of profound central nervous system dysfunction such as obtundation or unconsciousness may result in delayed treatment and underscores the importance for maintaining a high level of suspicion during athletic events [9].
Inaccurate Equipment Can Result in Misidentification
Rectal thermometers, such as the one seen here, are the only way of getting an accurate rectal temperature to recognize EHS.
The only accurate and practical prehospital method of core body temperature evaluation for EHS is to use a rectal thermometer, placed at a depth of 15 centimeters (about 6 inches) [10]. The National Athletic Trainers’ Association (NATA), like NAEMSP, similarly recommends that rectal thermometers be considered the gold standard for EHS assessment and therefore should be part of the EHS emergency treatment plan for athletic programs [11] . As such, EMS providers should be educated on these thermometers being used prior to ambulance arrival. Once inserted, the rectal thermometer should be left in place for continuous monitoring during cooling efforts and transport. Many rectal thermometers used in the hospital setting are only inserted 1.5 centimeters into the rectum and therefore are not accurate enough for EHS assessment [12]. Temporal artery thermometers, ear/tympanic membrane thermometers, and oral thermometers are not accurate in the detection of EHS and should not be used [13-15].
(A) Hospital thermometers probes (left) generally are unable to be inserted into the recommended depth of 15cm (B) Clockwise from left: Temporal artery surface thermometer, oral digital thermometer, tympanic membrane thermometer and forehead infrared thermometer. These devices should not used in the evaluation of EHS due to problems with accuracy.
Strategies for Rapid Cooling
This 50 Gallon tub is used at the Indianapolis Mini Marathon for Cold Water Immersion
Rapid cooling is the key management step of EHS. Rapid cooling should begin when the patient is symptomatic. Based on expert consensus, if the rectal temperature is greater than 40.5 °C (104.9 °F), Cold Water Immersion cooling should occur when available (see algorithm below), as it most expeditiously accomplishes rapid cooling. This involves placing the patient into a tub of ice water (with enough ice to maintain a water temperature of 10 °C / 50 °F ) and the body immersed in water from the neck down. Tubs of approximately 50-gallon capacity are generally sufficient for this task, though some programs prefer tubs of 150-gallon capacity [16]. Proper cooling techniques should result in a reduction of rectal temperature to less than 38.6 °C (101.5 °F) within 30 minutes.
Other alternatives include the use of a tarp (“tarp assisted cooling”), also filled with ice water, while the water is agitated continuously by responders to keep the cold water moving [17]. A similar technique involves using a fluid impervious body bag filled with ice water, which may be helpful in the hospital setting if no tub or tarp is available.
Other field methods of cooling
The use of ice packs placed close to arteries (neck, axilla, groin) has been taught for many years and may be one of the few practical options in an ambulance. However, this technique appears to have marginal cooling benefit when used alone and should not be used as the primary method of cooling whenever possible[18].
The US Army Training and Doctrine Command is a proponent of ice sheets as part of heat casualty response plan for trainees, which utilizes cotton sheets soaked in ice water and stored in coolers [19]. This requires placement of sheets onto as much bare skin as possible except for the face, and rotated with fresh sheets when the placed sheets start to feel warm. The technique is not as effective as cold water immersion [20].
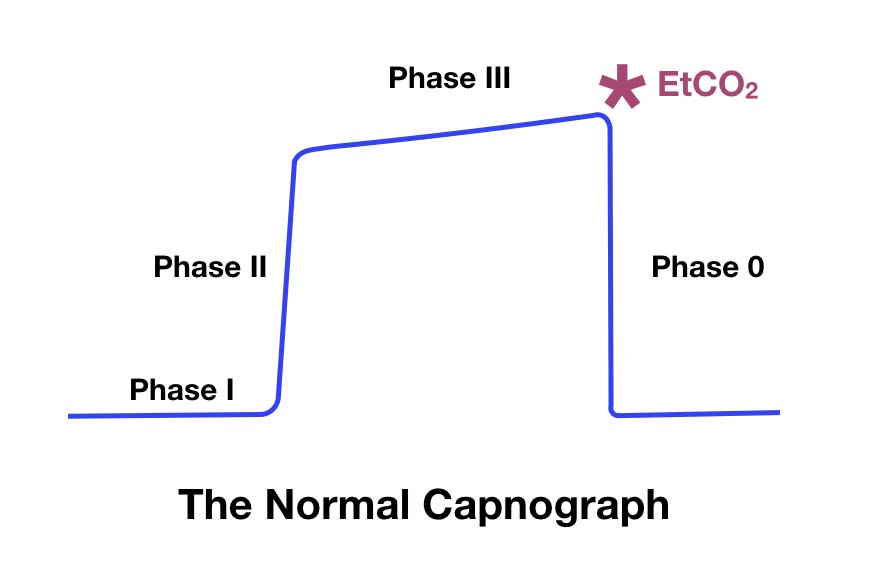
Recommended rectal temperature thresholds to start and stop Cold Water Immersion
Evaporative cooling, such as fanning a patient or even using the rotor wash from a helicopter, appears to be significantly slower than cold water immersion in reducing body temperature [21-22]. Evaporative cooling may also be less effective in high humidity situations.
While it may seem intuitive that chilled intravenous fluids would be helpful for rapid cooling, research in this area is limited. In a small study of healthy human volunteers, chilled saline of 4 °C (39.2 °F) decreased core body temperature by only 1 °C (1.8 °F) after 30 minutes [23]. Though using cold saline infusion in combination with other cooling modalities may improve patient outcomes [7].
Prehospital Protocol Considerations
Given the importance of rapid cooling in the setting of EHS, EMS protocols should consider prioritizing cold water immersion over transport if the equipment is available onsite; NAEMSP and NATA both recommend a “cool first, transport second” approach. Communication with the receiving hospital is essential, particularly if onsite cooling is unavailable as Emergency Departments may need to initiate cooling in non-traditional care areas such as a decontamination room. EMS providers should be reminded to consider other causes of collapse and confusion, including hypoglycemia and hyponatremia.
Prevention
Monitoring Wet Bulb Globe Temperature provides a real-time assessment of heat risk
The risk of EHS is increased in the setting of hot, humid conditions. Providers working at mass gathering or athletic events should evaluate event policies regarding adjustments to work/rest cycles, safety messaging, rest/sleeping facilities, provision of cooling devices (such as arm immersion cooling systems) and ensure appropriate EHS response equipment is available [24]. The Heat Index or Wet Bulb Globe Temperature are tools that are useful in developing an understanding of current or projected risk of heat related illness [25].
Conclusion
EHS can be effectively managed in the prehospital environment when recognized in a timely fashion. A high index of suspicion is needed anytime an athlete experiences CNS disturbance after doing physical activity: responders can be falsely reassured when the climate does not appear too warm, CNS disturbance is only mild or if the patient’s skin is not hot to the touch. A multidisciplinary approach should be taken to incorporate on-site medical personnel, such as athletic trainers, in developing protocols to ensure the coordinated management of EHS. Finally, EMS agencies should take steps to ensure the availability of equipment such as rectal thermometers and cold-water immersion supplies at local athletic centers, sporting events and military training venues.
References
1. Choudhary, E., & Vaidyanathan, A. (2014, December 12). Heat Stress Illness Hospitalizations — Environmental Public Health Tracking Program, 20 States, 2001–2010. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/ss6313a1.htm
2. Yeargin, S. W., Kerr, Z. Y., Casa, D. J., Djoko, A., Hayden, R., Parsons, J. T., & Dompier, T. P. (2016). Epidemiology of Exertional Heat Illnesses in Youth, High School, and College Football. Medicine & Science in Sports & Exercise, 48(8), 1523-1529. doi:10.1249/mss.0000000000000934
3. Yeargin, S. W., Dompier, T. P., Casa, D. J., Hirschhorn, R. M., & Kerr, Z. Y. (2019). Epidemiology of Exertional Heat Illnesses in National Collegiate Athletic Association Athletes During the 2009–2010 Through 2014–2015 Academic Years. Journal of Athletic Training, 54(1), 55-63. doi:10.4085/1062-6050-504-17
4. Centers for Disease Control and Prevention. (2010, August 20). Heat Illness Among High School Athletes --- United States, 2005--2009. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5932a1.htm
5. Armed Forces Health Surveillance Branch. (2019, April 1). Update: Heat Illness, Active Component, U.S. Armed Forces, 2018. Retrieved from https://www.health.mil/News/Articles/2019/04/01/Update-Heat-Illness
6. Sloan, B. K., Kraft, E. M., Clark, D., Schmeissing, S. W., Byrne, B. C., & Rusyniak, D. E. (2015). On-site treatment of exertional heat stroke. Am J Sports Med, 43(4), 823-9. doi:10.1177/0363546514566194
7. Belval, L. N., Casa, D. J., Adams, W. M., Chiampas, G. T., Holschen, J. C., Hosokawa, Y., … Stearns, R. L. (2018). Consensus Statement- Prehospital Care of Exertional Heat Stroke. Prehospital Emergency Care, 22(3), 392-397. doi:10.1080/10903127.2017.1392666
8. Roberts, W. O. (2006). Exertional Heat Stroke during a Cool Weather Marathon. Medicine & Science in Sports & Exercise, 38(7), 1197-1203. doi:10.1249/01.mss.0000227302.80783.0f
9. Hostler, D., Franco, V., Martin-Gill, C., & Roth, R. N. (2014). Recognition and Treatment of Exertional Heat Illness at a Marathon Race. Prehospital Emergency Care, 18(3), 456-459. doi:10.3109/10903127.2013.864357
10. Miller, K. C., Hughes, L. E., Long, B. C., Adams, W. M., & Casa, D. J. (2017). Validity of Core Temperature Measurements at 3 Rectal Depths During Rest, Exercise, Cold-Water Immersion, and Recovery. Journal of Athletic Training, 52(4), 332-338. doi:10.4085/1062-6050-52.2.10
11. Casa, D. J., DeMartini, J. K., Bergeron, M. F., Csillan, D., Eichner, E. R., Lopez, R. M., … Yeargin, S. W. (2015). National Athletic Trainers' Association Position Statement: Exertional Heat Illnesses. Journal of Athletic Training. doi:10.4085/1062-6050-50-9-07
12. Welch Allyn. (2018). Capturing Rectal Temperature. Retrieved from https://www.welchallyn.com/content/dam/welchallyn/documents/sap-documents/MRC/80022/80022620MRCPDF.pdf
13. Ronneberg, K., Roberts, W. O., McBean, A. D., & Center, B. A. (2008). Temporal Artery Temperature Measurements Do Not Detect Hyperthermic Marathon Runners. Medicine & Science in Sports & Exercise, 40(8), 1373-1375. doi:10.1249/mss.0b013e31816d65bb
14. Huggins, R., Glaviano, N., Negishi, N., Casa, D. J., & Hertel, J. (2012). Comparison of Rectal and Aural Core Body Temperature Thermometry in Hyperthermic, Exercising Individuals: A Meta-Analysis. Journal of Athletic Training, 47(3), 329-338. doi:10.4085/1062-6050-47.3.09
15. Mazerolle, S. M., Ganio, M. S., Casa, D. J., Vingren, J., & Klau, J. (2011). Is Oral Temperature an Accurate Measurement of Deep Body Temperature? A Systematic Review. Journal of Athletic Training, 46(5), 566-573. doi:10.4085/1062-6050-46.5.566
16. Zhang, Y., Davis, J., Casa, D. J., & Bishop, P. A. (2015). Optimizing Cold Water Immersion for Exercise-Induced Hyperthermia. Medicine & Science in Sports & Exercise, 47(11), 2464-2472. doi:10.1249/mss.0000000000000693
17. Hosokawa, Y., Adams, W. M., Belval, L. N., Vandermark, L. W., & Casa, D. J. (2017). Tarp-Assisted Cooling as a Method of Whole-Body Cooling in Hyperthermic Individuals. Annals of Emergency Medicine, 69(3), 347-352. doi:10.1016/j.annemergmed.2016.08.428
18. Gaudio, F. G., & Grissom, C. K. (2016). Cooling Methods in Heat Stroke. The Journal of Emergency Medicine, 50(4), 607-616. doi:10.1016/j.jemermed.2015.09.014
19. Training and Doctrine Command. (n.d.). Prevent of heat and cold casualties (TRADOC Regulation 350-29). Retrieved from Department of the Army website: https://adminpubs.tradoc.army.mil/regulations/TR350-29.pdf
20. Nye, E. A., Eberman, L. E., Games, K. E., & Carriker, C. (2017). Comparison of Whole-Body Cooling Techniques for Athletes and Military Personnel. Int J Exerc Sci, 10(2), 294-300. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5360373/
21. Armstrong, L. E., Crago, A. E., Adams, R., Roberts, W. O., & Maresh, C. M. (1996). Whole-body cooling of hyperthermic runners: Comparison of two field therapies. The American Journal of Emergency Medicine, 14(4), 355-358. doi:10.1016/s0735-6757(96)90048-0
22. Poulton, T. J., & Walker, R. A. (1987). Helicopter cooling of heatstroke victims. Aviat Space Environ Med, 58(4), 358-61.
23. Moore, T. M., Callaway, C. W., & Hostler, D. (2008). Core Temperature Cooling in Healthy Volunteers After Rapid Intravenous Infusion of Cold and Room Temperature Saline Solution. Annals of Emergency Medicine, 51(2), 153-159. doi:10.1016/j.annemergmed.2007.07.012
24. DeGroot, D. W., Kenefick, R. W., & Sawka, M. N. (2015). Impact of Arm Immersion Cooling During Ranger Training on Exertional Heat Illness and Treatment Costs. Military Medicine, 180(11), 1178-1183. doi:10.7205/milmed-d-14-00727
25. Casa, D. J., DeMartini, J. K., Bergeron, M. F., Csillan, D., Eichner, E. R., Lopez, R. M., … Yeargin, S. W. (2015). National Athletic Trainers' Association Position Statement: Exertional Heat Illnesses. Journal of Athletic Training. doi:10.4085/1062-6050-50-9-07
EMS MEd Editor : Maia Dorsett, MD PhD (@maiadorsett)




































![Pan et. al. Table 3 [Reference 7]](https://images.squarespace-cdn.com/content/v1/58174dbb6a496367e36143b1/1505327105970-YJPOUOUJET70KQTL4IBT/Pan_Table3.jpg)